Abstract
Introduction The prognosis of patients with very high-risk hematologic malignancies who have relapsed/refractory diseases or carrying very poor-risk gene mutations were dismal even after allogeneic hematopoietic stem cell transplantation. Donor lymphocyte infusion (DLI) is a promising prophylactic strategy for reducing relapse after transplant. However, DLI-associated graft-versus-host disease (GVHD) and non-relapse mortality (NRM) were still concerned, especially after allogeneic peripheral blood stem cell transplantation (allo-PBSCT). Therefore, prophylactic DLI should be safe with tolerable DLI-associated GVHD and NRM except for its anti-leukemia effect. To evaluate the safety and efficacy of prophylactic DLI for the very high-risk hematologic malignancies after allo-PBSCT, we performed a cohort study in 160 consecutive patients with hematological malignancies who received unmanipulated allo-PBSCT. DLI procedure was modified to use G-CSF mobilized peripheral progenitors instead of steady state lymphocytes and 4 to 6 weeks of immunosuppressant for prevention of DLI-associated GVHD. The outcomes of those very high-risk patients (group A: DLI group; group B: non-DLI group) and the patients without the very high-risk features (group C) who were not planned for prophylactic DLI were compared.
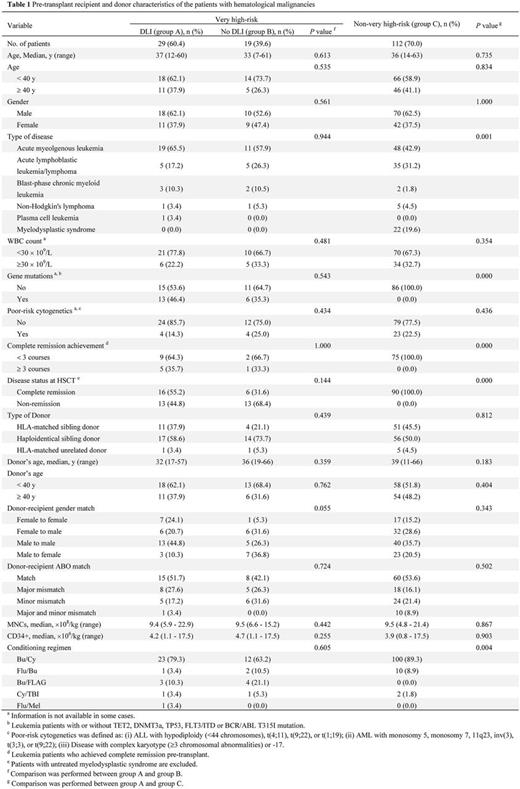
Patients and Methods The underlying diseases consist of acute myeloid leukemia (n = 78), myelodysplastic syndrome (n = 22), acute lymphoblastic leukemia/lymphoma (n = 45), chronic myeloid leukemia (n = 7), non-Hodgkin's lymphoma (n = 7), and plasma cell leukemia (n = 1). Sixty five patients (41.2%) received allo-PBSCT from HLA-matched sibling donors, 7 patients (4.4%) from matched unrelated donors, and 87 patients (54.4%) from haploidentical donors (Table 1). The very high-risk features were defined as 1) disease in non-remission state at time of transplant; 2) acute leukemia achieving complete remission (CR1) with 3 or more cycles of induction chemotherapy; 3) leukemia in CR1/CR2 carrying TP53, TET2 or DNMT3A gene mutation. Patients in CR with FLT3/ITD or BCR/ABL T315I gene mutation were enrolled due to the unavailability of effective targeted drugs. Prophylactic modified DLI was planned at 30 to 60 days post-transplant for all very high-risk patients with the absence of GVHD. The infusion was G-CSF mobilized peripheral progenitors from cryopreserved cell aliquots of the original graft. The trough concentration of CSA was maintained at 180 to 250 ng/mL for at least 4 to 6 weeks post-DLI and then discontinued within 2 weeks when no GVHD occurred. All the patients were followed-up for a median of 11.1 (0.5 - 29.7) months after transplant.
Results Prophylactic DLI was administered for 29 very high-risk patients (group A) at a median of 63 (25 - 176) days after transplant. The median numbers of mononuclear cells and CD3+ lymphocytes infused were 0.7 (0.1 - 1.4) × 108/kg and 18.5 (5.4 - 69.2) × 106/kg with a single dose. Nineteen patients (39.6%) with very high-risk features did not receive prophylactic DLI (group B) for the reasons of early relapse (n = 8), occurrence of GVHD (n = 8), and uncontrolled infections (n = 3). The cumulative incidence (CI) of grade II-IV acute GVHD at day 100 after transplant was 33.2% in group A, 38.0% in group B (p= 0.318), and 28.2% in group C (p= 0.746). The 2-year CI of chronic GVHD was 29.9% in group A, 15.8% in group B (p= 0.428), and 54.6% in group C (p= 0.255). The 2-year CI of relapse was 54.6% in group A, which was significantly lower than that in group B (68.4%, p= 0.019). The relapse-free survival in group A was superior to that in group B (37.3% vs . 24.6%, p = 0.032). In the very high-risk group of patients (group A and B), prophylactic DLI was correlated with a lower risk of relapse (p= 0.043, hazard ratio = 0.45). The 2-year CI of NRM in group A was not significantly different from that in group B (22.4% vs . 15.8%, p= 0.461) or group C (22.4% vs . 23.2%, p= 0.949). In addition, there was no significant difference in overall survival between group A and group B (48.6% vs . 35.1%, p = 0.134). The 6-month CI of CMV/EBV reactivations in group A was not significantly different from that in group B (p= 0.107 and p= 0.668) or group C (p= 0.130 and p= 0.596).
Conclusions This study showed that the prophylactic DLI after unmanipulated allo-PBSCT was well tolerated and effective for the patients with very high-risk hematologic malignancies in decreasing relapse without increasing the risks of GVHD and NRM.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal